EmerAX / TracLine LDP (088-90) positioned at C5 smoothly facilitates the recanalization of MCA occlusion.
Surgeon Introduction

Zhu Yong
Deputy Director of Neurology, Deputy Chief Physician
Shenzhen Guangming People’s Hospital
- Master of Medicine, graduated from Xiangya School of Medicine, Central South University, Australia
- Visiting scholar at the University of Sydney
- Senior member of Chinese Stroke Society
- Member of Cerebrovascular Disease Branch of Guangdong Medical Association
- Member of Ischemic Neurointervention Branch of Guangdong Stroke Society
- Member of Neurology Committee of Guangdong Primary Medicine Society
- Standing Committee of Interventional Radiology Committee of Shenzhen Health Management Society
- Director of Shenzhen Stroke Society
- Vice President of Integrated Chinese and Western Medicine Branch of Shenzhen Stroke Society
- Vice President of Intervention Branch of Shenzhen Stroke Society
- Member of Internal Medicine Committee of Shenzhen Medical Association
- Member of the Brain and Nerve Diseases Committee of Shenzhen Health Management Association
- Member of Interventional Medicine Branch of Shenzhen Hospital Association
- Youth Member of Neurologist Branch of Shenzhen Physician Association
Case information
Chief Complaint: Slurred speech and right limb weakness for 1 day.
Descrption of Present Illness:
The patient encountered slurred speech one day ago, with difficulty lifting his right upper extremity, trouble grasping, weakness in his right lower extremity, and difficulty walking without any apparent cause. He reported no physical twitching, urinary or fecal incontinence, or loss of awareness. The symptoms persisted and gradually worsened, prompting medical evaluation. Emergency cranial CT led to the admission diagnosis of “cerebral infarction.”
Past Medical History:
– Denies history of hypertension, hyperlipidemia, and diabetes mellitus.
– History of surgery on the right lower limb.
– Smoked for over 10 years, approximately half a pack per day.
– Does not consume alcohol.
Physical Examination:
– Blood Pressure: 153/108 mm Hg
– Mental Status: Conscious, slightly poor spirit, speech less clear and not fluent, but advanced cognitive functions are mostly normal.
– Pupils: Equal in size (approximately 3.0 mm in diameter) and responsive to light.
– Cranial Nerves: Symmetrical bilateral forehead lines, shallow right nasolabial fold, mouth angle deviates to the left when showing teeth, tongue extends midline.
– Motor Function: Left limb muscle strength at grade 5, right limb muscle strength at grade 4-. Normal muscle tone in all extremities.
– Reflexes: Bilateral tendon reflexes (++), no significant decrease in sensation, right side appears clumsy. Bilateral Babinski and Chaddock signs are negative. No signs of meningeal irritation.
– Scores: NIHSS score of 6 and MRS score of 3.
Diagnosis:
1. Acute cerebral infarction (left corona radiata).
2. Stage III hypertension.
Preoperative image
Cerebral CT at Our Hospital: Findings suggest the presence of a cerebral infarction in the left corona radiata.
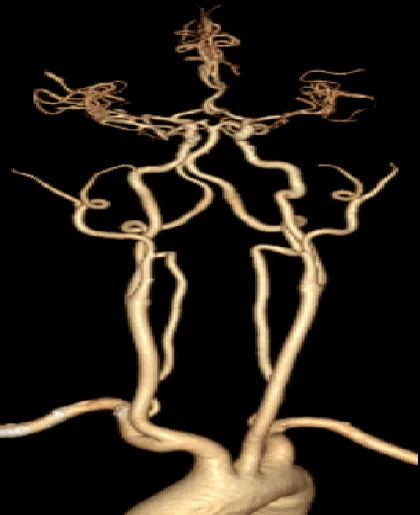
Head and neck CTA: Consideration of local mixed plaque and severe stenosis in the M1 segment of the left middle cerebral artery


Emergency cerebral perfusion: left frontal, parietal, temporal insula and basal ganglia decreased perfusion
Preoperative analysis
1. Indications for Surgery: The patient, a middle-aged male, presented with an extra-venous thrombolysis time window at admission. His NIHSS score was 6 points. Head and neck CTA combined with cerebral perfusion imaging suggested a mixed plaque with severe stenosis and occlusion in the left middle cerebral artery (MCA) M1 segment. There was also decreased perfusion in the left frontoparietal insula and basal ganglia, indicating cerebral arteriosclerosis. The mismatch volume was 86.4 ml, indicating a significant perfusion-diffusion mismatch.
2. Pathogenesis: The left MCA atherosclerosis has led to severe stenosis and occlusion. There is a high likelihood of thrombosis within the stenotic segment or distal to the stenosis.
3. Surgical Strategy: Based on head and neck CTA imaging data, the patient’s left MCA M1 segment is occluded, with fair imaging of M2 and M3 segments, suggesting collateral circulation compensation. The occlusion segment is short, with a low thrombus load. Therefore, a thrombectomy and angioplasty of the left MCA were performed.
4. The Procedure Involved the Following Interventional Instruments:
– Hemo’s EmerAX / TracLine LDP (088-90)
– 0.017″ microcatheter
– 200 cm 0.014″ micro guide wire
– 5F 125 cm intermediate guide catheter
– 3.0 * 25 mm Plug Removal Support
– 2.0 * 9 mm balloon dilatation catheter
Procedure

Left ICA angiography revealed occlusion of the M1 segment of the left MCA and compensatory feeding of the M2 and M3 segments of the left MCA via cortical branches.


The EmerAX / TracLine LDP (088-90) easily and smoothly reaches C5 under coaxial microguide wire, microcatheter and intermediate tube

The middle tube is placed in M1 via the EmerAX / TracLine LDP (088-90) large lumen distal access platform, and the microguide wire and microcatheter distal M2 confirm the true lumen

Partial restoration of blood flow was observed after the embolectomy stent was placed in M2 and released, and the EmerAX / TracLine LDP (088-90) remained stable.
Distal embolectomy stent protection followed by balloon (2.0-9mm) shaping, attention: slow expansion and withdrawal of pressure, gentle operation


After reconstruction, the distal blood flow was further restored, the middle tube negative pressure was started, and the thrombectomy stent was slowly withdrawn.


After 10 minutes, the blood flow was restored by EmerAX / TracLine LDP (088-90), distal diffusion was good, no residual stenosis and opacifier extravasation. After operation, the patient returned to the ICU.
Post-operative treatment
Intraoperative Management and Postoperative Care:
Intraoperative Management:
– Tirofiban administered at a rate of 7 ml/h during operation.
– Administration of Tirofiban halted 6 hours after bridging loading dose, which lasted for 36 hours.
Postoperative Medications:
– Butylphthalide
– Xuesaitong
– Ezetimibe
– Atorvastatin
Postoperative CT Scan:
– On second day post-operation, CT scan revealed a slight decrease in density and a slightly clearer edge in left coronal area.
– High density observed in anterior interhemispheric fissure cistern and left parietal lobe sulcus.
Prognosis:
– Patient discharged after 10 days.
– At discharge, patient was lucid and had good appetite and sleep quality. Speech had improved but remained unclear; further improvement in right limb weakness.
– EKG showed stable vital signs.
Physical Examination:
– Patient conscious and cooperative.
– Breath sounds in both lungs were clear without any dry or wet rales.
– No arrhythmias or obvious murmurs detected in any valvular area.
– Abdomen flat and soft, with no tenderness, and no edema in the lower limbs.
Neurological Examination:
– Patient alert and oriented with clear and fluent speech.
– Advanced intellectual activities normal.
– Pupils equal, round, and reactive to light, measuring about 3.0 mm in diameter.
– Bilateral frontal lines symmetrical, mouth angle not skewed, and extended tongue centrally positioned.
– Muscle strength was grade 5 in all four limbs, with normal muscle tone and bilateral tendon reflexes (++). Sensation was normal.
– Babinski and Chaddock signs were negative bilaterally.
Scores:
– NIHSS score: 0
– mRS score: 0
Case summary
In this case, the acute occlusion of the left MCA was caused by severe stenosis due to sclerosis. The EmerAX / TracLine LDP (088-90) proved particularly advantageous due to its soft transition segment at the tip end. This feature allows it to easily reach the C4/C5 segment of the ICA, significantly reducing the risk of vasospasm and vascular dissection, while providing stable overall support throughout the procedure. This is especially beneficial for complex type III aortic arches and tortuous ICA conditions. The patient greatly benefited from the EmerAX / TracLine LDP (088-90) due to its excellent navigability and robust support, ensuring a fast, safe, and smooth operation, and ultimately achieving a successful surgical outcome.
Product
About Hemo Bioengineering
Hemo Bioengineering Co., Ltd. (hereinafter referred to as “Hemo”) officially commenced operations in 2017. Hemo’s global headquarters are located in Singapore, with R&D centers in US, Singapore and China. The company maintains long-term collaborations with US-based R&D laboratories to ensure the design of new products aligns with cutting-edge global technologies.
Hemo is dedicated to leveraging global high-quality R&D, production, clinical, and academic resources to provide innovative vascular and neurological interventional products. These products aim to serve doctors and patients worldwide by offering comprehensive interventional treatment solutions for cerebrovascular diseases such as ischemic stroke, hemorrhagic stroke, and intracranial vascular stenosis.

